Times are difficult. Everyday things nobody used to bat an eye about are carefully evaluated and then executed with caution. With the interest of safety looming over our heads, it’s easy to get carried away and worry about every little detail. When faced with dilemmas of this sort, it is important to gauge the problem in question. Asses every variable and then come to a conclusion.
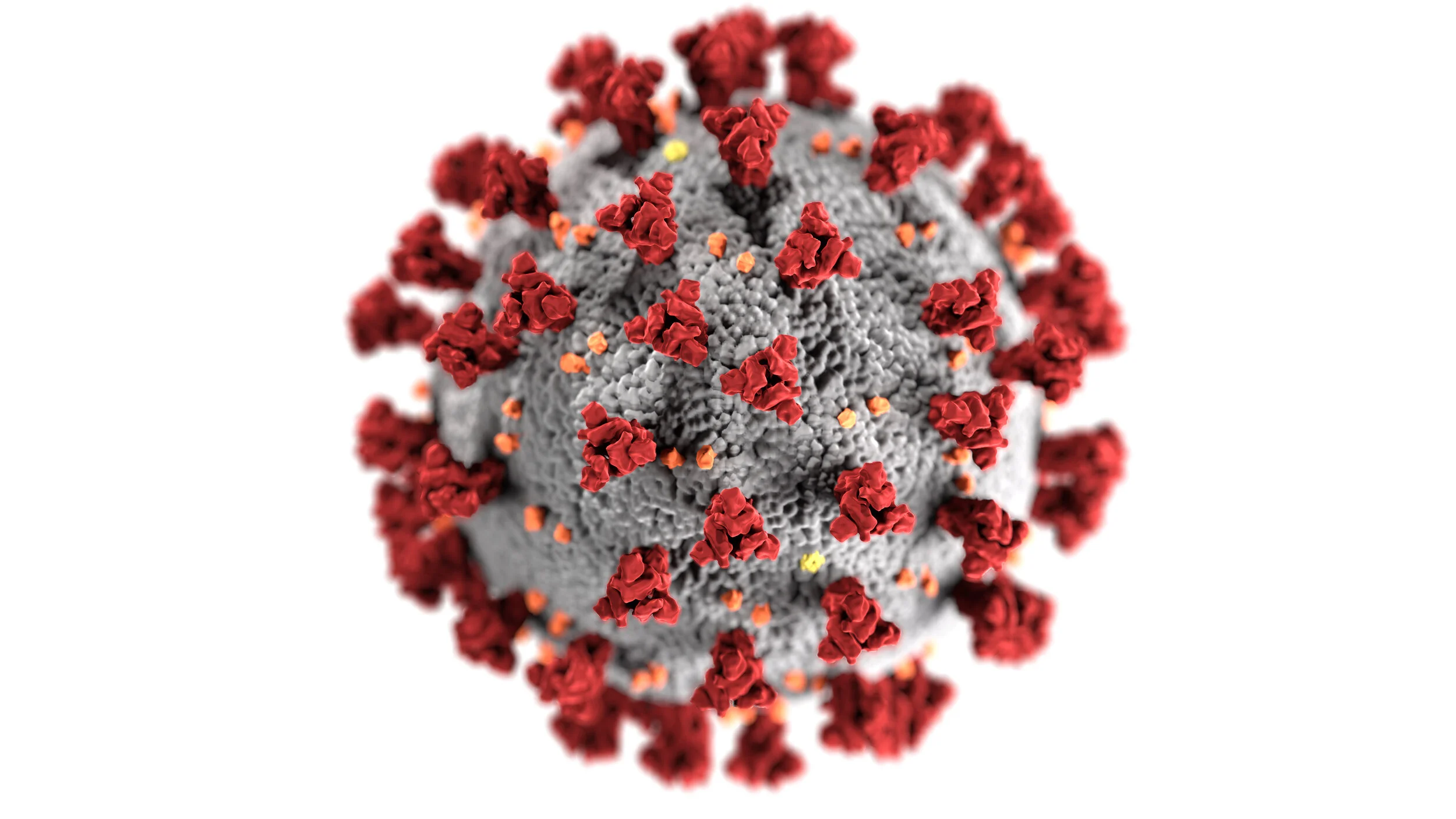
So, will the virus come in through my seemingly clean AC grill and infect me or not? It’s intuitive to think so as Air Conditioning systems (especially ones with central cooling/heating) usually have a centrally connected network of ducts. These ducts connect to air terminals across all conditioned spaces in the building. A corona virus particle which maybe as small as 120 nm may just fly across the return duct of an infected person’s room, make it all the way through the duct-work and into the spaces of innocent people. The idea isn’t a stretch by any means but the answer to the question is not a simple Yes or No.
Although there has been a report of an outbreak of corona virus disease (COVID-19) which affected 10 individuals belonging to 3 families all of whom had eaten at an air-conditioned restaurant in China, this transmission can be owed more to the airflow pattern rather than a transmission through the AC system. The virus is transmitted through droplets in the air. These droplets come from infected individuals when they cough or sneeze. This is exactly the reason you are expected to practice the “Vampire Cough” (covering the lower half of your face like a Vampire) when you cough or sneeze. Generally, the droplets do not tend to stay suspended for long and do settle onto surfaces where they can live for a rather long time. The nature of the surface and its surroundings determines how long the virus will actually stay alive if its not able to carry onto a host. If, however, a strong airflow pattern exists at the point of droplet emission, it is possible that the same can be carried over a farther distance before settling. This is the point of concern and where the significance of social distancing really comes into the picture. An affected individual will have a certain radius within which any other non-infected will be at risk of catching the disease through air. In a room where the air-conditioned air flow is strong, this radius can be even bigger. If proper distance is not maintained, several people in the room will be exposed to the same set of pathogens, which is why it would probably be better to avoid being in confined spaces with several people in a time that poses the danger of mass transmission. Rather than keeping dining tables far away from each other it would be better to avoid dining out in the first place. You can only have a romantic date if your date exists in the future!
In buildings with central air conditioning systems, there is a network of ducts that connects every room. Depending on the kind of system, chilled water or a refrigerant is pumped from the central units (usually placed on the roof or in the basement) to and from the smaller units placed on each floor which cater to separate spaces. Your building will probably also have an FAHU (Fresh Air Handling Unit) tasked with treating fresh air that comes into the building. In order to maintain comfortable conditions, building codes mandate HVAC systems to add a certain percentage of fresh air into the system with every cycle. The cooling of this air from outside temperature to comfortable levels will add extra load on the building’s system. Understandably, increasing the percentage of fresh air added will lead to increased running costs. Recirculating return air within the building is more energy efficient as the return air will only be hotter than the supply air by a few degrees. However, re-circulation does give rise to the potential danger of transmitting an unwanted particle through the system. In this way a virus particle can potentially pass through the entire structure and into new spaces.
Transmission in this manner can be avoided by setting the systems to use 100% fresh air. Isolation centers work on this principle. While regular residential and commercial spaces are set to operate with positive pressure, isolation wards have negative pressure. In a regular system, the amount of air supplied into the space will be more than the extract i.e. the air taken out, leaving a net positive pressure within the room. This practice prevents infiltration or untreated air coming into the space through gaps or holes. With negative pressure being maintained in isolation wards there is no question of air leaving the space through any opening. The negative pressure ensures that air can only pass into the space through an opening. If an infected individual were to sneeze or cough in such a room, releasing droplets with virulent particles into the air, such droplets would simply pass through the return ducts after which it will be treated. The presence of HEPA (high-efficiency particulate air) filters in such systems will ensure that such particles will not get recirculated in the system. In addition, isolation wards will usually be set to operate with 100 percent fresh air.
The point to note is that if a complete air change occurs, the chance for transmission is also slight. Several airlines also practice frequent air changes with frequencies closing even one air change every 5 minutes. This being said, it’s imperative to note that if you are seated next to an infected individual, the chance for contacting an infection is still very high.
To summarize, will any AC bring the virus into your home? No. Window or regular ductless split systems do not circulate air within the building and hence pose very little risk of spreading a disease-causing virus or bacteria through the air. With centrally conditioned systems, the case is not exactly the same. More variables come into the picture and we will only be able to comment with conclusive evidence when it comes out. Hence, such a scenario cannot be ignored.